你認識茲卡病毒嗎?儘管主要疫區在距離我們遙遠的中南美洲,而開幕在即的2016年巴西里約奧運,正是熱門疫區所在。在主張停辦奧運與續辦兩派人馬爭論不休的同時,有學者研究出新的發現,讓我們來看看是什麼?
加州大學舊金山分校與加州柏克萊大學的研究人員已經繪製出了茲卡病毒是如何感染發育中胎兒的路徑,並且已經發現一種抗生素可以阻斷這些感染路徑,至少在人體細胞培養中。
這些研究與發現,於7月18日刊登在Cell Host & Microbe期刊中,指出這類病毒,藉由斑蚊傳播並且導致一種稱為小頭畸形(Microcephaly)的胎兒畸形以及急性多發性神經炎(Guillain-Barré syndrome, GBS)等症狀,已傳遍南美與中美洲而且正朝著美國南部蔓延。小頭畸形症,推測病毒是通過在1-28週 (註1) 懷孕期內感染茲卡病毒的媽媽傳導給發育中的胎兒所引起,特徵是頭部小且腦部受損而導致精神與學習障礙,有時還帶點抽搐。
UCSF與UC Berkeley團隊發現,病毒會透過兩條潛在路徑來影響發育中的胎兒:懷孕初期所生成的胎盤以及懷孕中期才會生成的羊膜囊。在實驗室裡針對人體組織所作的研究發現,一種名為” 耐久霉素(duramycin)” 的較早期抗生素,阻斷了病毒複製出那些被認為要傳送到這兩條路徑的細胞。
“我們的論文顯示,耐久霉素有效地阻斷許多胎盤細胞類型與完整初期人體胎盤組織被來自目前拉丁美洲所爆發的當代茲卡病毒株中所分離出來的病毒感染;在那裡,懷孕期間感染茲卡病毒一直與小頭畸形等先天性缺乏症有關”,論文研究的共同作者Eva Harris,加州柏克萊大學公共衛生學院的一位傳染病學與疫苗學教授,這麼說道,”這表示耐久霉素或相似的藥可以有效減低或預防茲卡病毒從母體透過兩種潛在路徑傳染給胎兒並且防止相關的先天性缺陷”。
耐久霉素是一種由細菌生產去對抗其他細菌的抗生素。它常被用於動物,並且對於患有囊性纖維化的人尚在臨床實驗階段。近來的研究已經顯示在細胞培養實驗中它可以有效的對抗登革熱與西尼羅河病毒,也就是像茲卡這樣的黃病毒,以及絲狀病毒,像是伊波拉。
“非常少病毒能夠在懷孕期間延伸到胎兒並且造成先天性缺陷”,Lenore Pereira說道,他是病毒學家同時也是加州大學舊金山分校牙醫學院的細胞與組織生物學教授。要了解某些病毒是如何做這點是個非常重大的問題而且當媽媽受到感染時該如何保護胎兒們也許是該思考的最基本問題。
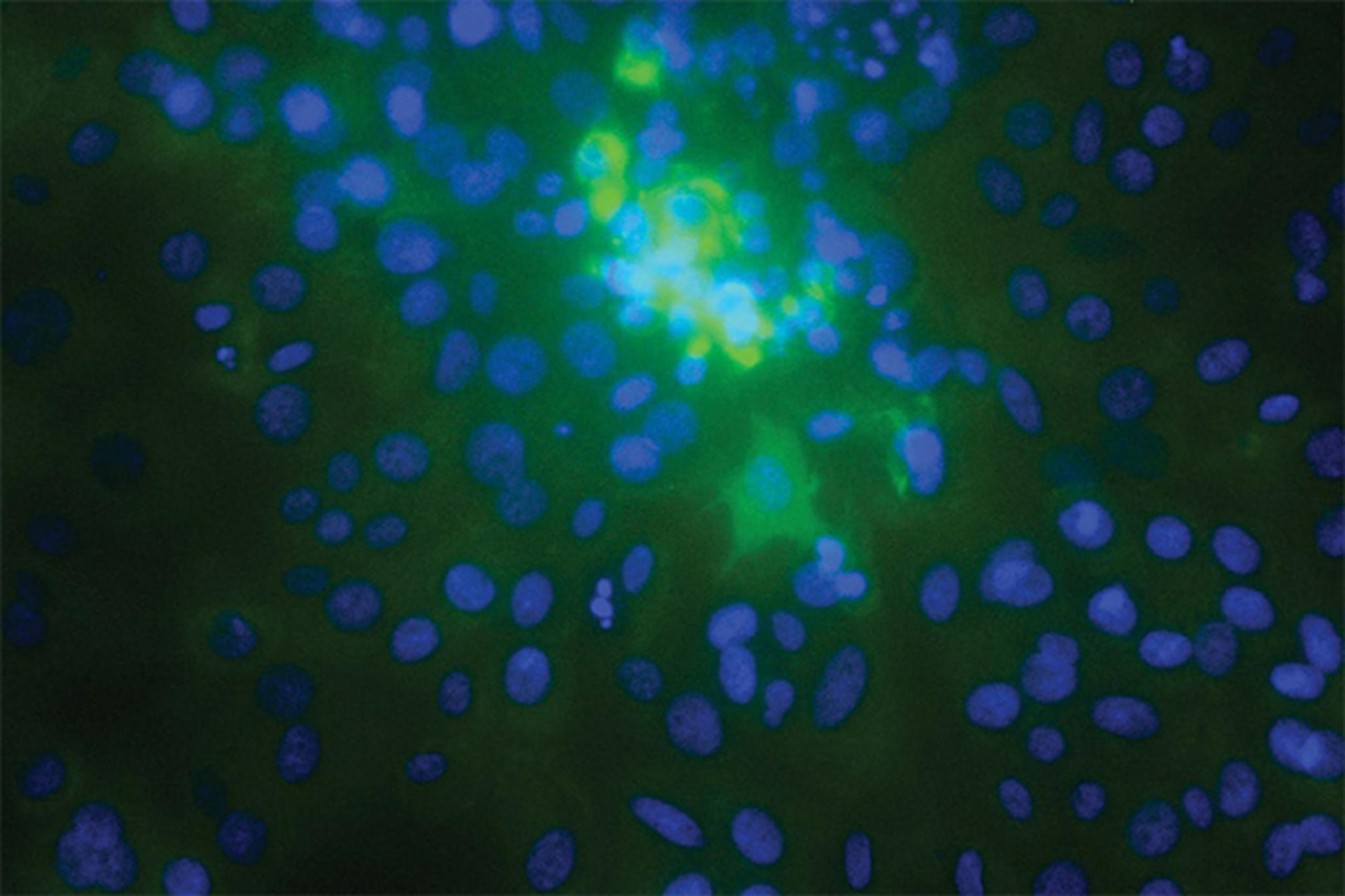
茲卡病毒,研究人員分別在分離的細胞中以及完整的組織外植體中檢驗,發現它會感染幾種不同的胎盤細胞類型,包含在胎盤內的細胞類型以及在胎盤外但在胎膜內的。科學家發現胎兒附近的羊膜上皮細胞特別容易受到茲卡病毒的感染。
“這意謂著細胞在仲介傳輸給胎兒中扮演著相當重大的角色,也支持著傳輸可以獨立地發生在胎盤膜之間,特別是在懷孕中後期的這項理論”Pereira說。 “最嚴重的先天性缺陷與茲卡感染相關 - 像是小頭畸形 - 似乎發生在女性於懷孕初期與中期受感染時。但也有可能在較小的範圍內,仍有些嚴重的先天性缺陷會發生當女性在懷孕後期時受感染。
本篇論文的其他作者包含了加州柏克萊大學的Henry Puerta-Guardo, Daniela Michlmayr以及Chunlin Wang,還有加州大學舊金山分校的Takako Tabata, Matthew Petitt以及June Fang-Hoover。
這項研究由美國國家衛生研究院(National Institutes of Health, NIH)轄屬機構美國國家過敏症與傳染病研究所(National Institute of Allergy and Infectious Diseases, NIAID)所資助。
註1:西方將孕程大致平均切成三期,前三個月,中間三個月,和後面三個月分別稱為first trimester、second trimester和third trimester。First trimester妊娠第一期(1-12週);Second trimester妊娠第二期(13-28週);Third trimester妊娠第三期(29-40週)。
本文由UC Berkeley的Robert Sanders在Jul. 18, 2016發表於UC官方網站
以下為原文:
Antibiotic may block Zika virus infection of fetus
UC San Francisco and UC Berkeley researchers have mapped out how the Zika virus infects the developing fetus, and have found an antibiotic that blocks these routes of infection, at least in human cell culture.
The findings, published today (July 18) in the journal Cell Host & Microbe, comes as the virus, spread by mosquitoes and linked to a fetal deformity called microcephaly as well as Guillain-Barré syndrome in adults, has spread throughout South and Central America and is heading toward the southern U.S. Microcephaly, presumably caused when the virus crosses from an infected mother to the growing fetus in the first two trimesters of pregnancy, is characterized by a small head and serious brain damage leading to physical and learning disabilities and sometimes convulsions.
The UCSF/UC Berkeley team found that the virus has two potential routes to the developing fetus: a placental route established in the first trimester, and a route across the amniotic sac that becomes available only in the second trimester. The study of human tissue in the laboratory found that an older-generation antibiotic called duramycin blocked the virus from replicating in cells that are thought to transmit it along both routes.
“Our paper shows that duramycin efficiently blocks infection of numerous placental cell types and intact first-trimester human placental tissue by contemporary strains of Zika virus recently isolated from the current outbreak in Latin America, where Zika virus infection during pregnancy has been associated with microcephaly and other congenital birth defects,” said study co-author Eva Harris, a professor of infectious diseases and vaccinology at UC Berkeley’s School of Public Health. “This indicates that duramycin or similar drugs could effectively reduce or prevent transmission of Zika virus from mother to fetus across both potential routes and prevent associated birth defects.”
Duramycin is an antibiotic that bacteria produce to fight off other bacteria. It is commonly used in animals and is in clinical trials for people with cystic fibrosis. Recent studies have shown it to be effective in cell culture experiments against dengue and West Nile virus, which are flaviviruses like Zika, as well as filoviruses, like Ebola.
“Very few viruses reach the fetus during pregnancy and cause birth defects,” said Lenore Pereira, a virologist and professor of cell and tissue biology in the UCSF School of Dentistry. “Understanding how some viruses are able to do this is a very significant question and may be the most essential question for thinking about ways to protect the fetus when the mother gets infected.”
The Zika virus, which the researchers examined in isolated cells and intact tissue explants, was found to infect several different placental cell types, including cell types within the placenta and outside the placenta in the fetal membranes. The scientists found that the epithelial cells of the amniotic membrane surrounding the fetus were particularly susceptible to Zika virus infection.
“This suggests that these cells play a significant role in mediating transmission to the fetus and supports the hypothesis that transmission could occur across these membranes independently of the placenta, especially in mid- and late gestation,” Pereira said. “The most severe birth defects associated with Zika infection — like microcephaly — seem to occur when a woman is infected in the first and second trimester. But there may be a range of lesser but still serious birth defects that occur when a woman is infected later in pregnancy.”
Other authors of the paper include Henry Puerta-Guardo, Daniela Michlmayr and Chunling Wang of UC Berkeley and Takako Tabata, Matthew Petitt and June Fang-Hoover of UCSF.
The research was funded by the National Institute of Allergy and Infectious Diseases.